Plantar Fasciitis
Plantar Fasciitis (or fasciopathy) is a condition of pain and tissue damage at the attachment of the plantar fascia to the underside of the calcaneus (heel bone).
Patients presenting with plantar fasciitis will usually describe pain when the foot hits the floor in the morning or after periods of inactivity. The pain usually settles down only to return at the end of the day.
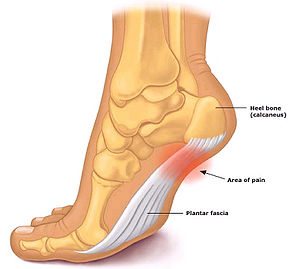
Anatomy
The plantar fascia is a band of connective tissue that runs along the sole from the heel to the ball of the foot. One of its main roles is to keep the bones and joints in position and enables us to push off from the ground. Bruising or overstretching this ligament can cause inflammation and heel pain. In many cases, plantar fasciitis is associated with a heel spur. Surprisingly, the spur itself does not cause pain, and may often be found in the other foot without symptoms.
Risk factors for Plantar Fasciitis
- Certain sports. Activities that place a lot of stress on the heel bone and attached tissue, i.e. running, dance and aerobics.
- Flat-footed or high arches. People with flat feet may have reduced shock absorption, increasing strain on the plantar fascia. High arched feet have tighter plantar tissue, leading to similar effects.
- Middle-aged or older. Heel pain tends to be more common with ageing as muscles supporting the arch of the foot become weaker, putting stress on the plantar fascia.
- Overweight. Weight places a greater mechanical load on the plantar fascia. There is evidence that overweight and inactivity lead to chemical damage to the plantar fascia, with a worsening of pain.
- Pregnancy. Weight gain, swelling and hormonal changes that accompany pregnancy may lead to mechanical overload of the plantar fascia.
- Being on your feet. People with occupations that require a lot of walking or standing on hard surfaces may suffer plantar fascia pain.
- Wearing shoes with poor arch support or stiff soles. Poorly designed shoes may contribute to problems.
How can you prevent Plantar Fasciitis?
- Maintaining a healthy weight to minimise the stress on the plantar fascia.
- Choosing supportive shoes. Avoiding stiletto heels and shoes with excessively low heels. Buying shoes with a low to moderate heel, good arch support and absorption. Not going barefoot, especially on hard surfaces.
- Not wearing worn-out runners. Replacing old runners before they stop supporting and cushioning the feet. If a sport involves a lot of running, replacing shoes after about 650 kilometres of use.
- Starting activity slowly. Warming up before starting any activity or sport, and starting a new exercise program slowly.
- Undertaking training prior to competition to ensure readiness to play.
- Allowing adequate recovery time between workouts or training sessions.
- Checking the sporting environment for hazards.
- Drinking water before, during and after play.
- Avoiding activities that cause pain.

What are the Signs and Symptoms of Plantar Fasciitis?
Pain is usually felt on the underside of the heel, and is often most intense with the first steps of the day or after rest. It is commonly associated with long periods of weight bearing or sudden changes in weight bearing or activity.
You may experience:
- Sharp pain in the inside part of the bottom of the heel, which may feel like a knife sticking into the bottom of the foot.
- Heel pain that tends to be worse with the first few steps after awakening, when climbing stairs or when standing on tiptoe.
- Mild swelling in the heel.
- Heel pain after long periods of standing or after getting up from a seated position.
- Heel pain after, but not usually during, exercise.
Immediate Management
Initial treatment includes gentle stretching of the Achilles tendon and plantar fascia, weight loss, taping, arch support and heel lifts. Difficult cases may be referred for physiotherapy. Physiotherapy includes myofascial release and scar tissue breakdown of the plantar fascia, and supervised stretching. A strengthening program for the calf muscles and small muscles of the foot is important. Be aware that this may increase soreness initially, but persistence should be rewarding.
Care should be taken to wear supportive and stable shoes. Patients should avoid open-back shoes, sandals, ‘flip-flops’, and any shoes without raised heels. A podiatrist can assist with plantar fasciitis and other foot and lower limb problems.
What range of treatment is available for Plantar Fasciitis?
For most people, the condition improves spontaneously within a year. Treatments that may help control symptoms include:
- Night splints and Cam Walkers (‘Moon Boots’). Your Podiatrist may recommend wearing a splint fitted to the calf and foot while sleeping. This holds the plantar fascia and Achilles tendon in a lengthened position overnight.
- Orthotics. Your Podiatrist may prescribe off-the-shelf or custom-fitted arch supports (orthotics) to help distribute pressure to the feet more evenly, and to stimulate the small foot muscles.
- Shockwave Therapy is high intensity ultrasound waves delivered in a non-invasive way. These sound waves are delivered through a special hand piece to treat heel spurs, plantar fasciitis and Achilles tendon problems.
- Low Level Laser Therapy. LLLT uses light energy to stimulate cells, helping them to function optimally, which in turn encourages the healing process. Once the photons find the injured tissues, they stimulate and energise the cells to repair and strengthen at a remarkably fast rate. Collagen production is stimulated so the ligaments and tissues grow stronger than with normal healing.
- Podiatry. Your Podiatrist can provide a range of aids and appliances to help with Plantar fasciitis as well as give instruction on a series of exercises to stretch the plantar fascia and Achilles tendon and to strengthen lower leg muscles, which stabilises the ankle and heel.
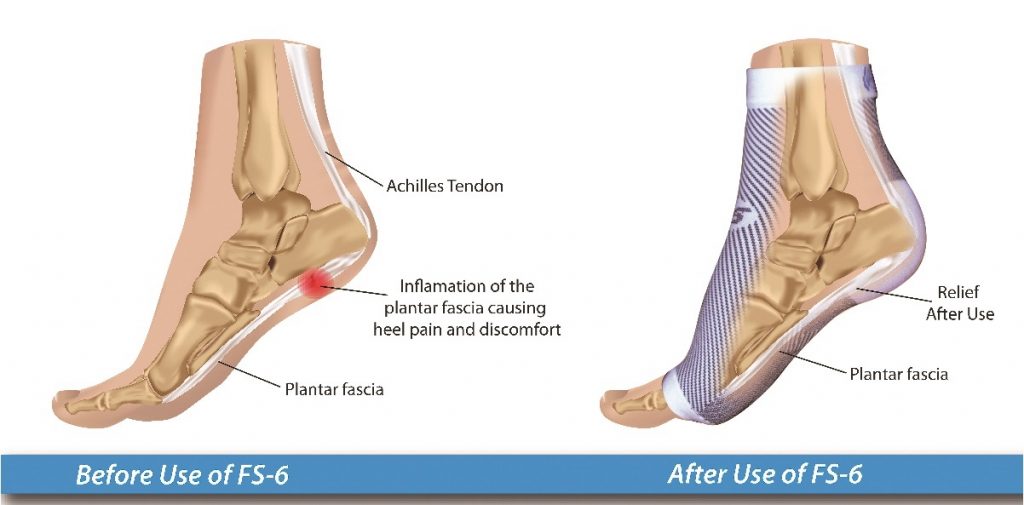
- Compression & Support Socks: Your Podiatrist might consider the benefit of added support, compression, enhanced circulation and stability offered by a compression sock.
- Strapping. Often professional strapping applied by a Podiatrist provides immediate relief of symptoms from Plantar Fasciitis. Often this is a good indicator of the benefit of more permanent and long term supportive measures, such as orthotics, for your feet in both alleviating the pain and preventing future problems and deterioration.
- Dry Needling. A fast, minimally invasive technique appears to provide long-term relief from plantar-fasciitis pain.
- Medication, injection therapy and surgery. These measures are for the most persistent cases, and do not replace the need for the treatment methods detailed above.

Shockwave Therapy & Plantar Fasciitis
The Foot and Ankle Clinic & Plantar Fasciitis
Podiatrists at The Foot and Ankle Clinic have vast experience in diagnosing and treating Plantar Fasciitis and typically treatment is very successful but involves a multifactorial approach. We also prescribe and supply a wide range of treatment aids to assist with rehabilitation and prevention of Plantar Fasciitis.
At the Foot and Ankle Clinic our highly qualified team of Podiatrists are all members of the Australian Podiatry Association and offer a combined 50 years’ experience. They are trained to diagnose and effectively treat Plantar Fasciitis via a range of treatments.
Put your feet in our hands! See us today in Chadstone, Moe, Sale, Traralgon, Warragul & Online Store and Retail Enquiries. NO REFERRAL NEEDED!.










