Foot and Ankle Arthritis
Arthritis is inflammation of one or more of your joints. It can cause pain and stiffness in any joint in the body and is very common in the small joints of the foot and ankle.
There are hundreds of forms of arthritis, many affecting the foot and ankle. All of them can lead to pain and major secondary complications making it difficult to walk and perform activities you enjoy.
Although there is no cure for arthritis, there are many treatment options available to slow the progress of the disease and relieve symptoms. With proper diagnosis, assessment and treatment, many people with arthritis are able to manage their pain, remain active, and lead fulfilling lives. Podiatrists at The Foot and Ankle Clinic are highly skilled and experienced at treating arthritic feet and ankles.
During standing, walking, and running, the foot and ankle provide support, shock absorption, balance, and several other functions that are essential for motion. There are 28 bones in the foot, and more than 30 joints that allow for a wide range of movement.
In many of these joints the ends of the bones are covered with articular cartilage that helps the bones glide smoothly over each other during movement. Joints are surrounded by a thin lining called the synovium. The synovium produces a fluid that lubricates the cartilage and reduces friction.
Tough bands of tissue, called ligaments, connect the bones and keep the joints in place. Muscles and tendons also support the joints and provide the strength to make them move.
Types of Arthritis
The major types of arthritis that affect the foot and ankle are osteoarthritis, rheumatoid arthritis, posttraumatic arthritis and gout.
Osteoarthritis
Osteoarthritis, is the most common and is a degenerative or “wear-and-tear” arthritis. This is usually a problem for many people after they reach middle age, but it may occur in younger people, too.
In osteoarthritis, the cartilage in the joint gradually wears away. As the cartilage wears away, it becomes frayed and rough, and the protective space between the bones decreases. This can result in bone rubbing on bone, and produce painful osteophytes (bone spurs).
In addition to age, other risk factors for osteoarthritis include obesity and family history of the disease and poor foot and alignment or biomechanics.
Osteoarthritis develops slowly, causing pain and stiffness that worsen over time.
Rheumatoid Arthritis
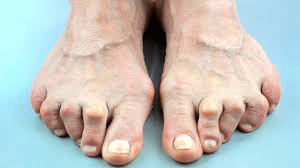
Rheumatoid arthritis is a chronic, systemic disease that can affect multiple joints throughout the body, and often starts in the foot and ankle. It usually affects the same joint on both sides of the body.
Rheumatoid arthritis is an autoimmune disease. This means that the immune system attacks its own tissues. In rheumatoid arthritis, immune cells attack the synovium covering the joint, causing it to swell. Over time, the synovium invades and damages the bone and cartilage, as well as ligaments and tendons, and may cause serious joint deformity and disability.
The exact cause of rheumatoid arthritis is unknown. Although it is not an inherited disease, researchers believe that some people have genes that make them more susceptible. There is usually a “trigger,” such as an infection or environmental factor, which activates the genes. When the body is exposed to this trigger, the immune system begins to produce substances that attack the joints.
The most common clinical presentation of Rheumatoid Arthritis in the feet is in the form of prominent 1st to joint (similar to bunions) along with the prominent metatarsal heads on the balls of the feet with reduced fatty tissue.
Juvenile rheumatoid arthritis (JRA), is the most common form of childhood arthritis. In most patients, the immunogenic associations, clinical pattern, and functional outcome of JIA are different from those of adult-onset RA.
Post-traumatic Arthritis
Post-traumatic arthritis can develop after an injury to the foot or ankle. Dislocations and fractures—particularly those that damage the joint surface—are the most common injuries that lead to post-traumatic arthritis. Like osteoarthritis, post-traumatic arthritis causes the cartilage between the joints to wear away. It can develop many years after the initial injury.
An injured joint is about seven times more likely than an uninjured joint to become arthritic, even if the injury is properly treated. In fact, following an injury, your body may actually secrete hormones that stimulate the death of your cartilage cells.
Gout
Gout is a painful inflammation of a joint. The big toe is the joint most commonly affected, although the hands, wrists, knees, ankles, elbows or any other joint can be affected.

Gout is the result of a build of waste material called uric acid, which forms tiny crystals in some of the joints of the body. Uric acid is normally found in the blood of all people, and comes from the breakdown of cells, DNA and from the food and drinks we consume each day.
Uric acid is mostly excreted by the kidneys. Too much uric acid builds up in the blood either because it is not excreted quickly enough or because too much is being produced. This excess can end up in the joints as crystals (called ‘urate’). These crystals can cause sudden and severe inflammation of the joint.
Gout is uncommon in women before the onset of menopause. It is more common in men than in women, and in older people than in younger people, but can affect anyone.
Arthritis Symptoms
The symptoms of arthritis vary depending on which joint is affected. In many cases, an arthritic joint will be painful and inflamed. Generally, the pain develops gradually over time, although sudden onset is also possible. There can be other symptoms, as well, including:
- Pain with motion
- Pain that flares up with vigorous activity
- Tenderness when pressure is applied to the joint
- Joint swelling, warmth, and redness
- Increased pain and swelling in the morning, or after sitting or resting
- Difficulty in walking due to any of the above symptoms
Physical Examination
Your Podiatrist will discuss your overall health and medical history and ask about any medications you may be taking. He or she will examine your foot and ankle for tenderness and swelling and ask questions to understand more about your symptoms. These questions may include:
- When did the pain start?
- Where exactly is the pain? Does it occur in one foot or in both feet?
- When does the pain occur? Is it continuous, or does it come and go?
- Is the pain worse in the morning or at night? Does it get worse when walking or running?
Your Podiatrist will also ask if you have had an injury to your foot or ankle in the past. If so, he or she will discuss your injury, including when it occurred and how it was treated.
Your doctor will also examine your shoes to determine if there is any abnormal or uneven wear and to ensure that they are providing sufficient support for your foot and ankle.
Gait analysis: During the physical examination, your Podiatrist will closely observe your gait (the way you walk). Pain and joint stiffness will change the way you walk. For example, if you are limping, the way you limp can tell your doctor a lot about the severity and location of your arthritis.
During the gait analysis, your Podiatrist will assess how the bones in your leg and foot line up when you walk, measure your stride, and test the strength of your ankles and feet.
Arthritis Tests
X-rays. These imaging tests provide detailed pictures of dense structures such as bone. An x-ray of an arthritic foot may show narrowing of the joint space between bones (an indication of cartilage loss), changes in the bone (such as fractures), or the formation of bone spurs.
Weight-bearing x-rays are taken while you stand. They are the most valuable additional test in diagnosing the severity of arthritis and noting any joint deformity associated with it. In arthritic conditions, if x-rays are taken without standing, it is difficult to assess how much arthritis is present, where it is located in the joint, and how much deformity is present. So, it is very important that, when possible, x-rays are taken standing.

Other imaging tests. In some cases, a bone scan, computed tomography (CT) scan, or magnetic resonance imaging (MRI) scan may be needed to determine the condition of the bone and soft tissues.
Laboratory tests. Your doctor may also recommend blood tests to determine which type of arthritis you have. With some types of arthritis, including rheumatoid arthritis, blood tests are important for an accurate diagnosis.
Your Podiatrist may refer you to a rheumatologist if he or she suspects rheumatoid arthritis. Although your symptoms and the results from a physical examination and tests may be consistent with rheumatoid arthritis, a rheumatologist will be able to determine the specific diagnosis. There are other less common types of inflammatory arthritis that will be considered.
Treatment
There is no cure for arthritis but there are a number of treatments that may help relieve the pain and disability it can cause.
Conservative / Nonsurgical Treatment
Initial treatment of arthritis of the foot and ankle is usually nonsurgical. Your Podiatrist may recommend a range of treatment options.
Lifestyle modifications. Some changes in your daily life can help relieve the pain of arthritis and slow the progression of the disease. These changes include:
- Minimizing activities that aggravate the condition.
- Switching from high-impact activities (like jogging or tennis) to lower impact activities (like swimming or cycling) to lessen the stress on your foot and ankle.
- Losing weight to reduce stress on the joints, resulting in less pain and increased function.
Physical therapy. Specific exercises can help increase range of motion and flexibility, as well as help strengthen the muscles in your foot and ankle. Your Podiatrist can help develop an individualized exercise program that meets your needs and lifestyle.
Although physical therapy often helps relieve stress on the arthritic joints, in some cases it may intensify joint pain. This occurs when movement creates increasing friction between the arthritic joints. If your joint pain is aggravated by physical therapy, your Podiatrist will stop this form of treatment.
Aids & Appliances. Using or wearing a brace—such as an ankle-foot orthosis (AFO)-may help improve mobility. In addition, wearing shoe inserts (orthotics) or custom-made shoes with stiff soles and rocker bottoms can help minimize pressure on the foot and decrease pain. In addition, if deformity is present, a shoe insert may tilt the foot of ankle back straight, creating less pain in the joint. Cushioned insoles are often helpful to customized to accommodate lesions and provide pressure relief.

Medications. Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, can help reduce swelling and relieve pain. In addition, cortisone is a very effective anti-inflammatory agent that can be injected into an arthritic joint. Although an injection of cortisone can provide pain relief and reduce inflammation, the effects are temporary. The Foot and Ankle Clinic’s Musculoskeletal Podiatrist, Dr. James Ferrie has great success using a range of more natural Tissue Regeneration Therapy (TRT) treatment modalities.
Surgical Treatment
Your Podiatrist may recommend surgery if your pain causes disability and is not relieved with nonsurgical treatment. The type of surgery will depend on the type and location of the arthritis and the impact of the disease on your joints. In some cases, your doctor may recommend more than one type of surgery.

At the Foot and Ankle Clinic our highly qualified team of Podiatrists are all members of the Australian Podiatry Association and offer a combined 50 years’ experience. They are trained to diagnose and effectively treat Foot and Ankle Arthritis via a range of treatments.
Put your feet in our hands! See us today in Chadstone, Moe, Sale, Traralgon, Warragul & Online Store and Retail Enquiries. NO REFERRAL NEEDED!.


