Rheumatoid Arthritis
Rheumatoid arthritis is a chronic, systemic disease that can affect multiple joints throughout the body, and often starts in the foot and ankle. It usually affects the same joint on both sides of the body.
Rheumatoid arthritis is an autoimmune disease. This means that the immune system attacks its own tissues. In rheumatoid arthritis, immune cells attack the synovium covering the joint, causing it to swell. Over time, the synovium invades and damages the bone and cartilage, as well as ligaments and tendons, and may cause serious joint deformity and disability.
The exact cause of rheumatoid arthritis is unknown. Although it is not an inherited disease, researchers believe that some people have genes that make them more susceptible. There is usually a “trigger,” such as an infection or environmental factor, which activates the genes. When the body is exposed to this trigger, the immune system begins to produce substances that attack the joints.
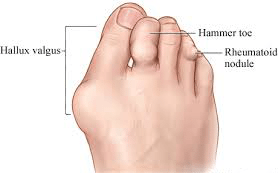
The most common clinical presentation of Rheumatoid Arthritis in the feet is in the form of prominent 1st to joint (similar to bunions) along with the prominent metatarsal heads on the balls of the feet with reduced fatty tissue.
Symptoms of rheumatoid arthritis
The symptoms of arthritis vary depending on which joint is affected. In many cases, an arthritic joint will be painful and inflamed. Generally, the pain develops gradually over time, although sudden onset is also possible. There can be other symptoms, as well, including:
- Pain with motion
- Pain that flares up with vigorous activity
- Tenderness when pressure is applied to the joint
- Joint swelling, warmth, and redness
- Increased pain and swelling in the morning, or after sitting or resting
- Difficulty in walking due to any of the above symptoms
Physical Examination
Your Podiatrist will discuss your overall health and medical history and ask about any medications you may be taking. He or she will examine your foot and ankle for tenderness and swelling and ask questions to understand more about your symptoms. These questions may include:
- When did the pain start?
- Where exactly is the pain? Does it occur in one foot or in both feet?
- When does the pain occur? Is it continuous, or does it come and go?
- Is the pain worse in the morning or at night? Does it get worse when walking or running?
Your Podiatrist will also ask if you have had an injury to your foot or ankle in the past. If so, he or she will discuss your injury, including when it occurred and how it was treated.
Your doctor will also examine your shoes to determine if there is any abnormal or uneven wear and to ensure that they are providing sufficient support for your foot and ankle.
Gait analysis: During the physical examination, your Podiatrist will closely observe your gait (the way you walk). Pain and joint stiffness will change the way you walk. For example, if you are limping, the way you limp can tell your doctor a lot about the severity and location of your arthritis.
During the gait analysis, your Podiatrist will assess how the bones in your leg and foot line up when you walk, measure your stride, and test the strength of your ankles and feet.
Tests
X-rays. These imaging tests provide detailed pictures of dense structures such as bone. An x-ray of an arthritic foot may show narrowing of the joint space between bones (an indication of cartilage loss), changes in the bone (such as fractures), or the formation of bone spurs.

Weight-bearing x-rays are taken while you stand. They are the most valuable additional test in diagnosing the severity of arthritis and noting any joint deformity associated with it. In arthritic conditions, if x-rays are taken without standing, it is difficult to assess how much arthritis is present, where it is located in the joint, and how much deformity is present. So, it is very important that, when possible, x-rays are taken standing.
Other imaging tests. In some cases, a bone scan, computed tomography (CT) scan, or magnetic resonance imaging (MRI) scan may be needed to determine the condition of the bone and soft tissues.
Laboratory tests. Your doctor may also recommend blood tests to determine which type of arthritis you have. With some types of arthritis, including rheumatoid arthritis, blood tests are important for an accurate diagnosis.
Your Podiatrist may refer you to a rheumatologist if he or she suspects rheumatoid arthritis. Although your symptoms and the results from a physical examination and tests may be consistent with rheumatoid arthritis, a rheumatologist will be able to determine the specific diagnosis. There are other less common types of inflammatory arthritis that will be considered.
Treatment
There is no cure for arthritis but there are a number of treatments that may help relieve the pain and disability it can cause.
Conservative / Nonsurgical Treatment
Initial treatment of arthritis of the foot and ankle is usually nonsurgical. Your Podiatrist may recommend a range of treatment options.
Lifestyle modifications. Some changes in your daily life can help relieve the pain of arthritis and slow the progression of the disease. These changes include:
- Minimizing activities that aggravate the condition.
- Switching from high-impact activities (like jogging or tennis) to lower impact activities (like swimming or cycling) to lessen the stress on your foot and ankle.
- Losing weight to reduce stress on the joints, resulting in less pain and increased function.
Physical therapy. Specific exercises can help increase range of motion and flexibility, as well as help strengthen the muscles in your foot and ankle. Your Podiatrist can help develop an individualized exercise program that meets your needs and lifestyle.
Although physical therapy often helps relieve stress on the arthritic joints, in some cases it may intensify joint pain. This occurs when movement creates increasing friction between the arthritic joints. If your joint pain is aggravated by physical therapy, your Podiatrist will stop this form of treatment.
Aids & Appliances. Using or wearing a brace—such as an ankle-foot orthosis (AFO)-may help improve mobility. In addition, wearing shoe inserts (orthotics) or custom-made shoes with stiff soles and rocker bottoms can help minimize pressure on the foot and decrease pain. In addition, if deformity is present, a shoe insert may tilt the foot of ankle back straight, creating less pain in the joint. Cushioned insoles are often helpful to customized to accommodate lesions and provide pressure relief.

Medications. Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, can help reduce swelling and relieve pain. In addition, cortisone is a very effective anti-inflammatory agent that can be injected into an arthritic joint. Although an injection of cortisone can provide pain relief and reduce inflammation, the effects are temporary. The Foot and Ankle Clinic’s Musculoskeletal Podiatrist, Dr. James Ferrie has great success using a range of more natural Tissue Regeneration Therapy (TRT) treatment modalities.
Surgical Treatment
Your Podiatrist may recommend surgery if your pain causes disability and is not relieved with nonsurgical treatment. The type of surgery will depend on the type and location of the arthritis and the impact of the disease on your joints. In some cases, your doctor may recommend more than one type of surgery.
At the Foot and Ankle Clinic our highly qualified team of Podiatrists are all members of the Australian Podiatry Association and offer a combined 50 years’ experience. They are trained to diagnose and effectively treat rheumatoid arthritis via a range of treatments.
Put your feet in our hands! See us today in Chadstone, Moe, Sale, Traralgon, Warragul & Online Store and Retail Enquiries. NO REFERRAL NEEDED!.


